Is ‘The Butcher of New England’ Harming Patients with Undisclosed Conflicts of Interest?

Migraine is a common, debilitating condition that is notoriously difficult to treat1. While conventional treatments offer a poor effectiveness versus safety profile, acupuncture has been demonstrated to be at least as effective if not more effective than medication with far fewer side-effects2. For this reason, acupuncture is recommended in official evidence-based clinical guidelines such as the UK’s NICE Guidelines for Headaches.
However, Harvard neurologist Paul G. Mathew, who appropriately refers to himself as ‘The Butcher of New England’, seems to have a different opinion on the matter. In his recent blog post on the Harvard Health blog, which was riddled with questionable puns but largely devoid of demonstrable familiarity with the research literature on the subject under discussion, Dr Mathew argued that the benefits of acupuncture were small while the evidence for conventional treatments strong, that physical therapy is a great alternative to drugs even when it doesn’t work, and ended with a questionable anecdote pointing to an undisclosed financial conflict of interest, rather than a good-willed desire to inform patients on their treatment options, as a possible motivation for steering migraine sufferers away from a treatment with a proven record of efficacy and safety.
Modest at Best
Dr Mathew’s discussion of the literature on treatments for migraines was on the whole anecdotal and unreferenced, leading one to ask what exactly was the point of writing the post in the first place. (Get it? Point? POINT?! It’s a pun on acupuncture. Two can play this game).
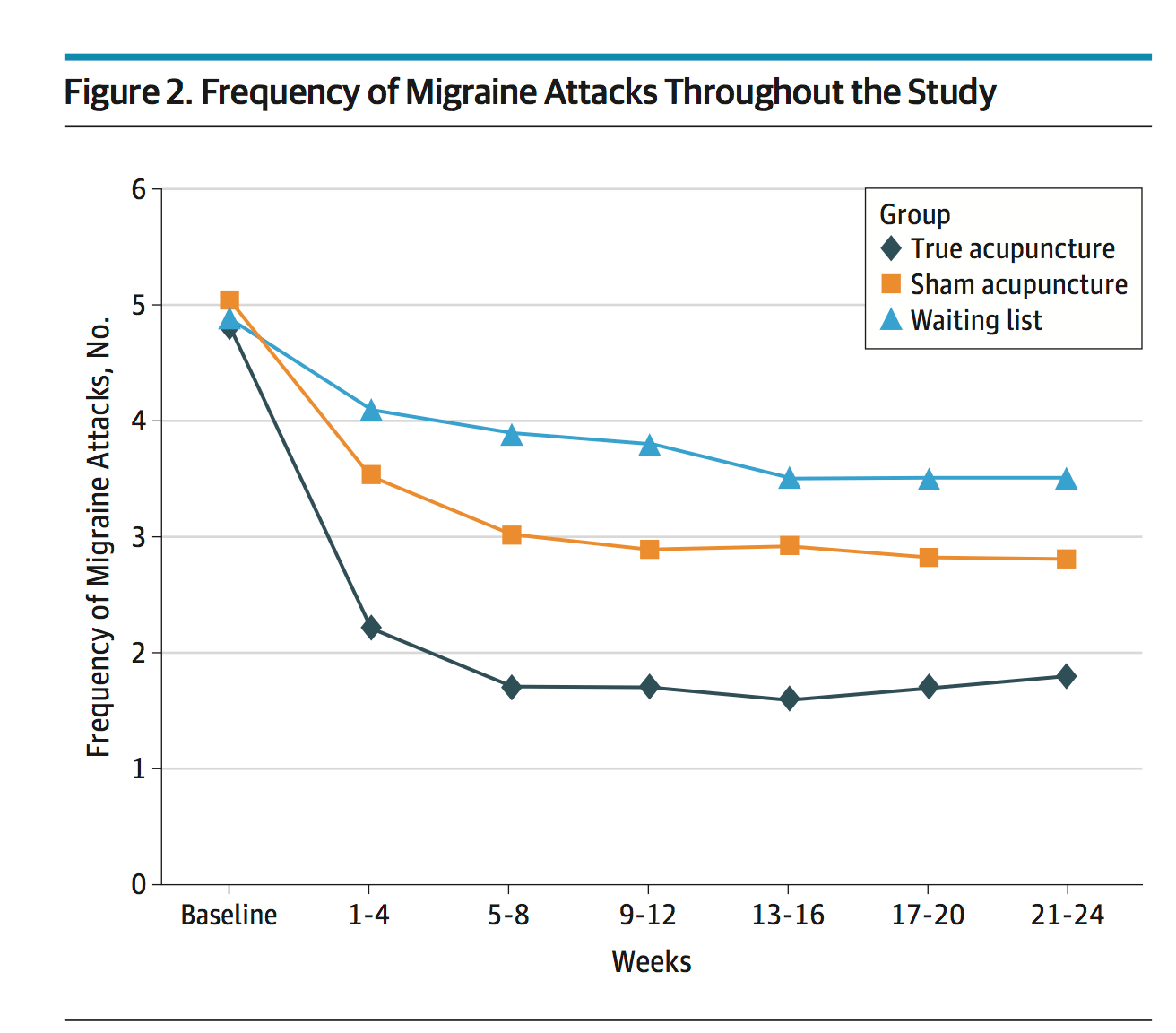
However, in an uncharacteristic move, Dr Mathew dabbled with using an actual citation to support his prose, referring to a recent clinical trial on acupuncture for migraine3. According to Dr Matthew: “Twelve weeks after treatment, the acupuncture group had on average 3.2 fewer attacks per month, the sham acupuncture group had 2.1 fewer attacks per month, and the wait-list group had 1.4 fewer attacks per month. These results are modest at best.”
Zhao, L., Chen, J., Li, Y., Sun, X., Chang, X., Zheng, H., et al. (2017). The Long-term Effect of Acupuncture for Migraine Prophylaxis. JAMA Internal Medicine, 177(4), 508–8. http://doi.org/10.1001/jamainternmed.2016.9378
So compared to sham needling, which is an active control with specific effects in the treatment of migraine4, true acupuncture was significantly more effective at reducing migraines at all time points while sham acupuncture was not significantly different from the waitlist control. Of course, normally, evidence-based practitioners prefer to use systematic reviews where available over individual studies. The most recent Cochrane review found that for reduction in headaches, acupuncture was associated with an effect size of 0.19 compared to active sham needling control 5, which to compare is greater than the effect size of SSRIs compared to placebo.6 Compared to usual care, the effect size is -0.56 in favor of acupuncture.
At 16 weeks, 200mg/day of Topiramate is associated with a reduction of 1.08 migraines per month7, whereas acupuncture has a 1.10 migraine reduction compared to sham needling.
Another migraine treatment, Botox injections, has even weaker support for its use. The PREEMPT trials, which were multi-armed Phase III trials funded by Allergan, the makers of Botox, found the following results for reduction in headaches per month: at 24 weeks, the Botox group had 5.2 fewer attacks and the placebo group had 4.9 fewer attacks, a difference of less than half a headache per month. At 56 weeks, the Botox group had 7.4 fewer attacks and the placebo group had 7.5 fewer attacks, a difference of precisely zero. Nada. Zilch.
So, Dr Mathew, if you describe the difference in reduction of headaches between acupuncture and active sham needling to be “modest at best,” then precisely how would describe the total lack of difference in headache reduction with Botox compared to placebo?
Butchering the Evidence on Standard Treatment
What’s interesting about the drugs used in the prevention of migraine, whether it’s an ACE inhibitor, alpha-blocker, beta-blocker, SSRI, serotonin agonist or tricyclic antidepressant, is that they all have something in common: none of them are actually migraine medications. They all fall into the category of ‘off-label prescribing.’ That’s when a drug approved for one use, such as an anti-depressant, is used for another entirely different use, such as migraine prevention, which it hasn’t been licensed or approved for. This situation arises because there aren’t really any medications that work very well for preventing migraines. Since this is pretty much common knowledge amongst clinicians, it was particularly surprising that as Dr Mathew argued against using acupuncture while pointing to evidence of its efficacy, he claimed that there’s good evidence for standard treatment, without pointing to any data at all.
Dr Mathew, not to be slowed down by actually reading the literature before summarizing it, tells us: “In general, the effectiveness of standard treatment (medication and injectable therapies) is supported by much stronger scientific evidence than acupuncture, including large clinical trials with thousands of subjects.” Fascinating. A 2015 meta-analysis8 of all drugs for the prevention of migraine, which included 126 randomized placebo-controlled clinical trials, found that the number of participants included in the studies was 112 on average, ranging from 9 to 783, making one wonder, pray tell, exactly which clinical trials with ‘thousands of subjects’ providing strong ‘scientific evidence’ for treating migraines with drugs Dr Mathew is referring to . . .
The results of this review are as follows: most of the drugs that are regularly used have no effectiveness beyond placebo. Drugs with at least 3 trials that were more effective than placebo for episodic migraines were as following:
– Amitriptyline: SMD: -1.2 (-1.7 to -0.82)
– Flunarizine: -1.1 headaches/month (-1.6 to -0.67)
– Fluoxetine: SMD: -0.57 (-0.97 to -0.17)
– Metoprolol: -0.94 headaches/month (CI -1.4 to -0.46)
– Pizotifen: -0.43 headaches/month (CI -0.6 to -0.21)
– Propranolol: 1.3 headaches/month (-2.0 to -0.62)
– Topiramate: -1.1 headaches/month (-1.9 to -0.73)
– Valproate: -1.5 headaches/month (-2.1 to -0.8)
So the studies on drugs that reported the results in terms of headaches per month had about the same advantage or perhaps less over placebo pill as acupuncture had over active sham control. And since the drugs were compared to an inert placebo and the acupuncture was compared to an active control, then it’s likely that acupuncture’s effectiveness is underestimated.
If that were the case, we’d expect acupuncture to outperform drugs when tested head to head, which is precisely what the literature shows.
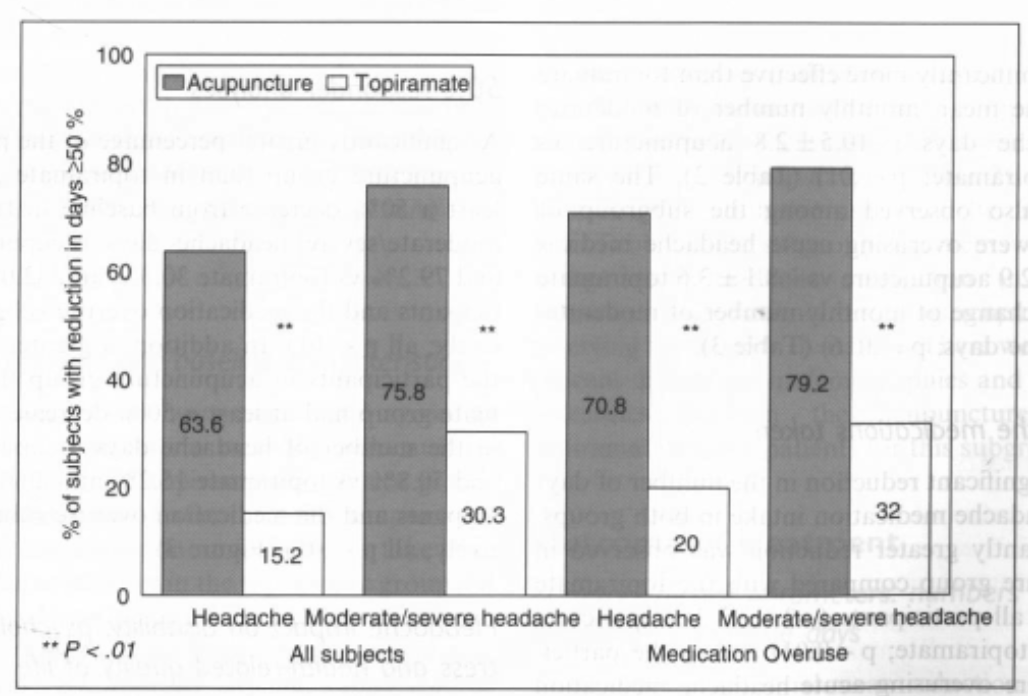
A randomized trial of acupuncture versus topiramate9, an anticonvulsant often used to treat migraines, demonstrated that acupuncture resulted in a significantly larger decrease in moderate/severe headaches (from 20.2 down to 9.8 versus 19.8 to 12 in the topiramate group). Additionally, acupuncture was more effective than topiramate for all secondary outcomes, such as pain intensity and quality of life. While adverse events occurred in 66% of the topiramate group, they only occurred in 6% of the acupuncture group, demonstrating a far superior benefit to risk profile for acupuncture.
Yang, C.-P., Chang, M.-H., Liu, P.-E., Li, T.-C., Hsieh, C.-L., Hwang, K.-L., & Chang, H.-H. (2011). Acupuncture versus topiramate in chronic migraine prophylaxis: a randomized clinical trial. Cephalalgia : an International Journal of Headache, 31(15), 1510–1521. http://doi.org/10.1177/0333102411420585
A 2013 study evaluating acupuncture vs valproic acid, another anti-epileptic drug, showed that at 6 months, pain intensity was lower in the acupuncture group, pain relief was greater, and the acupuncture group was taking significantly less acute medication (Rizatriptan). The rate of adverse events in the group given valproic acid was 47.8%; in the acupuncture group it was 0%.10
A recent Cochrane Systematic review confirms the findings of these studies. Compared to drugs, acupuncture is associated with -0.49 fewer migraine attacks at 8 weeks, -0.32 fewer migraines at 4 months, and -0.31 migraines 3.5 to 6 months after randomization compared to drugs. All results are statistically significant.
While self-styled acupuncture “Skeptics” (those who argue that acupuncture doesn’t work regardless of considerable evidence to the contrary) are quick to point out that head to head comparisons are biased because they are unblinded, researchers and clinical experts are quicker to point out that so is real life, where the patients are. Acupuncture’s superiority over sham and its many known biochemical mechanisms demonstrate specific effects. But of course, all of this is purely academic; head to head studies are the ones that tell you which treatments are most likely to benefit real patients in the real world comparing the treatment options that they are actually faced with, provided in the way that they would actually receive the treatment. The best evidence shows that acupuncture is more effective than drugs.
Side-effects?
“Side effects are not just limited to medications; procedures can also have negative effects,” Dr Mathew reminds us. Excellent point! According to an analysis of the safety and tolerability of Botox for chronic migraine, adverse events (AEs) were reported in a whopping 74% of those who received Botox. In fact, neck pain is such a common side-effect of the treatment that it results in unblinding in trials, as subjects know whether or not they’ve received the real deal based on how much pain they’re in afterwards.
Serious adverse events, which “were any that resulted in death, a life-threatening event, hospitalization (initial or prolonged), disability, a congenital anomaly or a medical event that could require medical or surgical intervention to prevent the above outcomes” was reported in 5.4% of those who were injected with Botox. The most common serious AE was (wait for it . . .) migraine. It’s unclear whether the common occurrence of migraines triggered by Botox treatment were classed as serious AE’s simply by causing disability or if a significant number of test subjects had migraines caused by Botox that were so severe they required hospitalization. Either way, causing serious migraines seems like sort of a counter-productive effect for a migraine treatment.
So what the data suggests is that not only does Botox not seem to reduce migraines compared to placebo, but the data shows that it actually causes them.11
After recommending against acupuncture based on a high-quality study that supports its efficacy, Dr Mathew has this advice for those who want to steer away from medication: “For those averse to medications, physical therapy is a great alternative — one based on actual human anatomy and scientific principles. My patients often complain that they do not feel significantly better after the five to 10 sessions of physical therapy that insurance companies typically approve. I advise them that the true benefit of physical therapy comes when the stretching and strengthening routines taught by the therapist are continued at home on a long-term basis.”
So physical therapy is ‘a great alternative’, even though a recent systematic review failed to show any effect on reducing migraines compared to control12 and even when his patients are telling him that it’s not working.
What would possibly compel Dr Mathew to write this?
The literature shows that acupuncture is an effective and safe treatment for migraine prophylaxis; indeed, it is one of the only ones clinical experts know of. It is more effective than sham needling, demonstrating specific effects and it’s more effective and safer than drugs, demonstrating that it should be offered as a first-line treatment and often is.
So why would Dr Mathew write a largely unreferenced blog post on Harvard’s Health Blog based on anecdote, opinion and conjecture that’s directly contradicted by the medical literature?
A possible clue comes at the finale of the piece, where we learn that a) Dr Mathew provides Botox injections for migraines, b) that he trains others to perform the procedure and c) that he thinks it’s appropriate to mock patients about how painful this procedure is (the safety data confirms that pain is a common result of the treatment and teasing patients about it just seems cruel).
Ok, so he’s a bit biased. He provides Botox and wants to rib the competition. Not very professional, appropriate or ethical, but we all get our kicks in different ways. It’s not like he’s received payment from Allergan, I mean that would be highly unethical not to mention totally inappropriate to write something so libelous and inaccurate without making his conflicts of interest crystal clear.
Just to double-check, I headed over to ProPublica and it would seem that Dr Mathew has indeed received money from Allergan, the makers of Botox.
I suppose we’ll never know if Dr Mathew would have taken it upon himself to steer patients away from a safe and effective treatment for a debilitating neurological condition towards a treatment that suffers from lack of evidence and a risky side-effect profile if he wasn’t financially incentivized to do so. One wonders if it is even appropriate for someone who is receiving money from the pharmaceutical industry to be writing about a non-pharmacological treatment such as acupuncture at all when they apparently lack any familiarity with the subject matter.
But one thing is crystal clear: Harvard, for the sake of public health and academic integrity, a highly visible conflict of interest declaration needs to be added to the top of this ‘blog post’ post-haste.
1 Jackson, J. L., Cogbill, E., Santana-Davila, R., Eldredge, C., Collier, W., Gradall, A., et al. (2015). A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache. PLoS ONE, 10(7), e0130733. doi.org/10.1371/journal.pone.0130733.s001
2 Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., et al. (2016). Acupuncture for the prevention of episodic migraine. (K. Linde, Ed.). Chichester, UK: John Wiley & Sons, Ltd. doi.org/10.1002/14651858.CD001218.pub3
3 Zhao, L., Liu, J., Zhang, F., Dong, X., Peng, Y., Qin, W., et al. (2014). Effects of Long-Term Acupuncture Treatment on Resting-State Brain Activity in Migraine Patients: A Randomized Controlled Trial on Active Acupoints and Inactive Acupoints. PLoS ONE, 9(6), e99538. doi.org/10.1371/journal.pone.0099538.s002
4 Appleyard, I., Lundeberg, T., & Robinson, N. (2014). Should systematic reviews assess the risk of bias from sham–placeboacupuncture control procedures? European Journal of Integrative Medicine, 6(2), 234–243. doi.org/10.1016/j.eujim.2014.03.004
5 Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., et al. (2016). Acupuncture for the prevention of episodic migraine. (K. Linde, Ed.). Chichester, UK: John Wiley & Sons, Ltd. doi.org/10.1002/14651858.CD001218.pub3
6 Jackson, J. L., Cogbill, E., Santana-Davila, R., Eldredge, C., Collier, W., Gradall, A., et al. (2015). A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache. PLoS ONE, 10(7), e0130733. doi.org/10.1371/journal.pone.0130733.s001.
7 Jackson, J. L., Cogbill, E., Santana-Davila, R., Eldredge, C., Collier, W., Gradall, A., et al. (2015). A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache. PLoS ONE, 10(7), e0130733. doi.org/10.1371/journal.pone.0130733.s001
8 Jackson, J. L., Cogbill, E., Santana-Davila, R., Eldredge, C., Collier, W., Gradall, A., et al. (2015). A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache. PLoS ONE, 10(7), e0130733. doi.org/10.1371/journal.pone.0130733.s001
9 Yang, C.-P., Chang, M.-H., Liu, P.-E., Li, T.-C., Hsieh, C.-L., Hwang, K.-L., & Chang, H.-H. (2011). Acupuncture versus topiramate in chronic migraine prophylaxis: a randomized clinical trial. Cephalalgia : an International Journal of Headache, 31(15), 1510–1521. doi.org/10.1177/0333102411420585
10 Facco, E., Liguori, A., Petti, F., Fauci, A. J., Cavallin, F., & Zanette, G. (2013). Acupuncture versus valproic acid in the prophylaxis of migraine without aura: a prospective controlled study. Minerva Anestesiologica, 79(6), 634–642.
11 Diener, H. C., Dodick, D. W., Turkel, C. C., Demos, G., DeGryse, R. E., Earl, N. L., & Brin, M. F. (2014). Pooled analysis of the safety and tolerability of onabotulinumtoxinA in the treatment of chronic migraine. European Journal of Neurology, 21(6), 851–859. doi.org/10.1111/ene.12393
12 Luedtke, K., Allers, A., Schulte, L. H., & May, A. (2016). Efficacy of interventions used by physiotherapists for patients with headache and migraine—systematic review and meta-analysis. Cephalalgia : an International Journal of Headache, 36(5), 474–492. doi.org/10.1177/0333102415597889

