Professor Ernst, a few questions about the new NICE guidelines
Dear Professor Ernst,
I appreciate you’re busy, but I was wondering if you could explain a few things to me. As the only professor of complementary medicine on the planet, you have unique insight and perspective on the new updates to the NICE Guidelines for low back pain. I understand that you expressed that the removal of the recommendation for acupuncture is good news for patients and indeed for society! That is very exciting! Yay!
But there were a few things I didn’t understand and I was wondering if you could clarify. First, you seem to approve of the recommendations of exercise, talking therapy, and patient education, even though none of these were more effective than sham/placebo. But I thought you said that if an intervention doesn’t outperform sham, it doesn’t really work. It’s just working through placebo and non-specific effects and thus it shouldn’t be offered. So why is it good to recommend these and not recommend acupuncture?
Second, it looks like the NICE made a bit of a boo boo. Acupuncture really did outperform sham for pain relief and some other things. Does the new evidence change your opinion? Or does your opinion stand regardless of any new information?
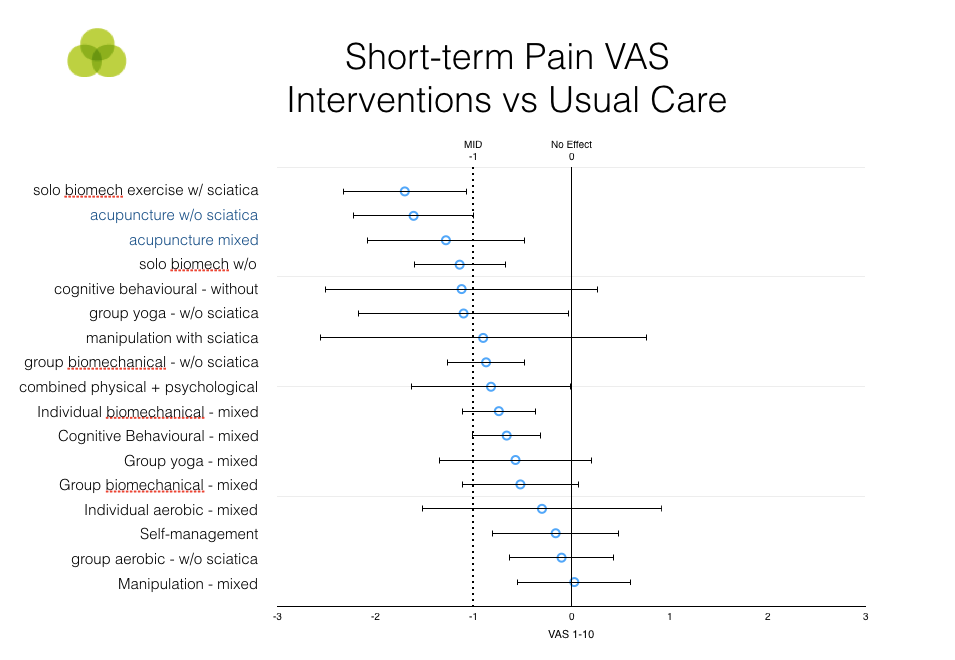
Finally, I understand that you share the opinion that acupuncture is just a theatrical placebo and I wondered if you could put that into perspective regarding the results below from NICEs evidence review.
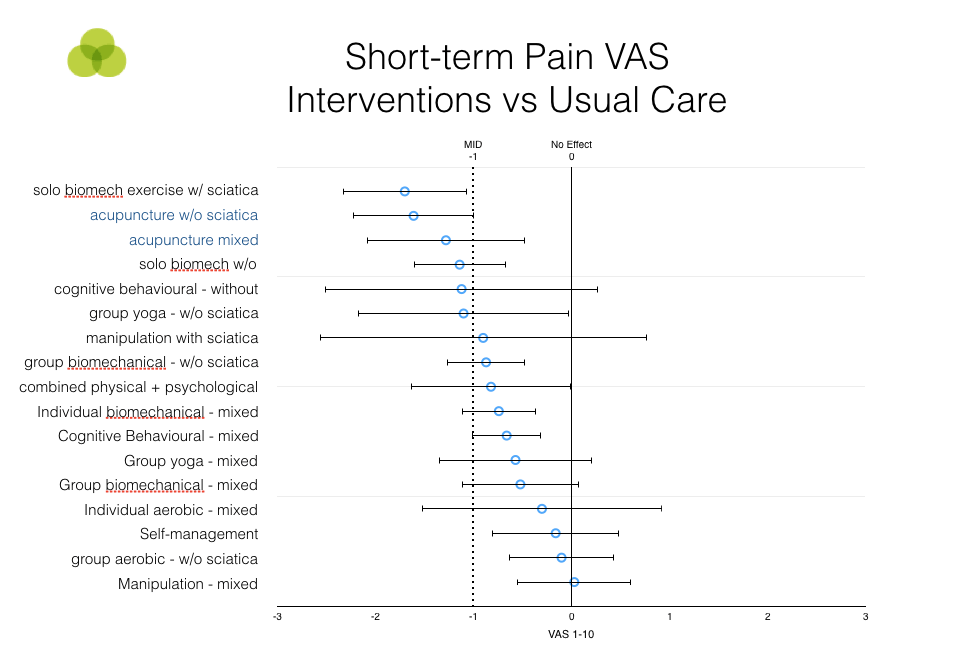
These results show that acupuncture was just about the most effective therapy of all the interventions reviewed by NICE for short-term pain relief. I understand that this is just one comparison, but a similar picture emerges for other measures. And even if it didn’t, ‘pain relief’ is probably a pretty important outcome measure for interventions to do with back pain.
Now, if acupuncture is ‘just a placebo’ as you say, then how does it get its placebo effects to be so much bigger than all of these other treatments (which were all recommended in the NICE guidelines even though some had no demonstrated effectiveness or efficacy), including ‘combined physical + psychological’ interventions. I mean, specifically, can you explain the mechanism? Because it seems a pretty neat trick! I mean, should we really not give patients the option of pain relief because of the remote possibility that the effects aren’t specific and offer them other, less effective treatments that have no demonstrated specific effects to speak of themselves?
And is it really more likely that acupuncture is wonderfully effective for pain relief but works only through placebo and empathy rather than working through a combination of non-specific, placebo and copious well documented specific effects? I mean, I accept that your explanation is possible, but is it really the most likely?
I’m also very interested in your thoughts about some of the other issues with the guidelines, that is, when you have time.
Curiously,
Mel

