What is the ‘Science-based’ treatment for the prevention of migraine?

Dear Science Based Medicine,
Over the years, I’ve followed your work with great interest in an effort to better understand ‘real’ medicine and how it is that treatments can consistently do well in trials and yet, according to ‘Science,’ not really work at all. It’s been very informative and I think I’m getting the hang of it.
While I’m pretty clear on what Science Based Medicine recommends against (pretty much anything that seems silly to the authors), I am more or less in the dark as to what it does recommend. It’s almost as if your site should be called ’Definitely not science-based medicine’ since that’s the preferred topic.
But I’m sure the public would be really interested to know, with real patients in the real world, which treatments does Science Based Medicine actually recommend? Because this is a very large topic, let’s specifically take the example of migraine prevention, partly because Dr Novella is a neurologist so he has clinical expertise here and partly because you specifically recommend against acupuncture, even when it outperforms other treatments. So I think it would help me, not to mention the public and healthcare policy makers, who also recommend acupuncture1, to understand if acupuncture is not a ‘science-based’ treatment for migraine, what in your estimation is?
What is ‘Science Based’ Medicine?
For those who are unfamiliar, a helpful place to begin our discussion is with what it means for medicine to be ‘Science based’ vs ‘Evidence based,’ which is the dominant paradigm in medicine. What follows is a genuine attempt to accurately summarise the SBM position (no intended straw men here) but I welcome clarification and correction, where needed.
In 2015, Dr Novella gave a talk on this very subject entitled ‘Science-Based Medicine: Beyond Integrated Medicine’, where he explained what Science Based Medicine is and how it goes a much needed step beyond Evidence Based Medicine.
He described ‘science’ in terms of five intellectual virtues, not specific to science, but emblematic of science, as follows:
1) Reasonably accounts for all available evidence. “What that means is that you can’t just pick and choose the evidence that you want. You have to account for all the evidence that’s available.”
2) Utilizes valid and internally consistent logic. “If you make an internally inconsistent logical statement, you’re not going to be led to a valid conclusion.”
3) Intellectually thorough, rigorous and methodical
4) Reasonably fair and unbiased in judgments
5) Adheres to standards of ethics and professionalism
When describing Evidence Based Medicine, in contrast, Dr Novella explained that EBM ‘assumes that products and practices that work and are safe are better than those that do not work or are unsafe.’ If you’re a patient, doctor or healthcare policy maker, you might be thinking this sounds like a pretty good way to go. But unfortunately while this approach may lead to safe and effective treatment options, it wouldn’t be appropriately labeled ‘science-based’ and would demonstrate a sad lack of critical thinking.
The main problem with the EBM approach, Dr Novella points out, is that it ignores ‘prior probability’ and does not adequately consider the ‘big picture’ of the entire literature. In other words, in randomized clinical trials, patients might have excellent results from a treatment like, say, acupuncture compared to usual care, pharmaceuticals, even sham needling. But if you don’t stop to consider how silly acupuncture seems in theory to a conventionally trained doctor, then you might incorrectly recommend it when you could recommend treatments that don’t work as well but seem more rational because they involve chemicals.
So EBM’s main weakness, according to SBM, is that it doesn’t go far enough, which is to say that it currently focuses too much on clinical evidence (how treatments effect patients), comparative effectiveness (which treatments work better than others) and safety and not enough on logic and prior probability (which treatments in theory should work). “Good science considers both.”
“Reasonably accounts for all available evidence”

The first virtue of Science Based Medicine, and the one that according to Science Based Medicine most distinguishes it from plain old Evidence Based Medicine, which is too focused on unscientific things like clinical evidence for what works and minimizes harm to patients, is that it “reasonably accounts for all available evidence. What that means is that you can’t just pick and choose the evidence that you want. You have to account for all the evidence that’s available.”
This approach sounds reasonable, if not a bit less relevant to patients than EBM.
So what I don’t understand, and hopefully you can provide some insight, is in the 2013 opinion piece, ‘Acupuncture is a Theatrical Placebo’, Colqhoun and Novella write that the number one thing NOT relevant to the discussion as to whether acupuncture is effective is the basic science research into acupuncture’s biochemical and neurological mechanisms: “We see no point in discussing surrogate outcomes, such as functional magnetic resonance imaging studies or endorphin release studies, until such time as it has been shown that patients get a useful degree of relief.” In other words, they only want to look at clinical evidence of their choosing, and completely ignore the entirety of the basic science literature for acupuncture. This approach is precisely the thing they accuse EBM of doing and what they claim makes them superior and more ‘Science’-based than their medical colleagues. When it’s pointed out that the clinical evidence for acupuncture is moderate to strong for dozens of clinical conditions2, they explain the results through placebo, non-specific effects, and regression to the mean (aspects of all treatments), having deemed the mechanism literature irrelevant.
What the basic science literature tells us is that acupuncture needling functions at least in part as a mechanical stimulus that results in a number of local and central effects (‘local’ being where you’re inserting the needle and ‘central’ being in the brain and spinal cord, both clinically helpful!). It causes fibroblasts (cells responsible for communication, remodeling and healing of the fascia) to stretch and degranulate, releasing a number of signaling molecules that act on local afferent nerves, which are more dense at acupuncture points.3 It also initiates purinergic signaling through the release of ATP and adenosine, which provides local anti-inflammatory effects as well as binding to local afferents that carry central signals. Interestingly, this release was found at an acupuncture point but not at the control point, lending support for specific effects.4
Downstream of the purines, other biochemicals involved in disease resolution, such as nitric oxide,5 BDNF6 and CGRP7 are released and regulated. Furthermore, unlike traditional ‘placebos’ that are known (sometimes but not always) to result in endorphin release, acupuncture, but not sham acupuncture needling, has been shown to increase receptivity to endorphins in the brain.8
So how is leaving out this literature consistent with considering all available evidence? Isn’t this the complete diametric opposite of your position to reasonably account for all available evidence and not rely solely on clinical evidence? A recent review of all available systematic review evidence (which Harriet Hall recently referred to as ‘cherry-picking,’ suggesting she may want a refresher on what the term means) found moderate or high-quality evidence that acupuncture provides a ‘useful degree of relief’ for 46 different conditions.9 On what grounds can you declare that this is entirely due to placebo if you consider the basic science literature on the physiological and biochemical effects of needling irrelevant? Is this internally logical, consistent, unbiased and ethical?
Equally, we could look at the other available treatments for migraine prophylaxis, at least some of which Dr Novella and others at SBM presumably recommend. Looking at the most common treatments for migraine prophylaxis, what does the basic science research say about beta-blockers for migraine? Is migraine caused by an over-activation of the sympathetic nervous system, such that chemically castrating this system is a logical recourse? Or anti-epileptics such as topiramate and valproate? Can you point me to the basic science research that demonstrates how these work for migraine? Do you test your migraine patients for serotonin deficiency before putting them on SSRI’s and pizotifen? Do drugs have biological plausibility for any condition no matter how they work because they’re drugs? If so, is that really scientific?
Or might this concept of ‘biological plausibility,’ the key feature that separates Science Based Medicine from the majority of mainstream medicine that just ‘doesn’t get it,’ actually be a subjective judgment based on what you choose to read?
‘Utilizes valid and internally consistent logic’
‘If you make an internally inconsistent logical statement, you’re not going to be led to a valid conclusion.’
The second virtue of Science, and Science Based Medicine by extension, is that it utilizes valid and internally consistent logic. I agree that logical consistency is a very helpful concept when studying medicine. Of course, as pointed out previously, one might ask how classifying all basic science research into acupuncture as irrelevant to a discussion of its mode of action can be considered internally consistent and logical, but I’m sure a valid explanation is forthcoming.
But let’s take another simple example of what is usually meant by ‘logical consistency.’ Let’s say you have a treatment that we’ll call Treatment A and you test it against another treatment, which we’ll call Treatment B. We might test these two against each other and discover that patients who were given Treatment A were significantly more likely to have a 50% reduction in their migraines than those given Treatment B. We could summarise these results by saying that Treatment A is more effective than Treatment B.
Further, if Treatment B is a sugar pill controlling for the effects of placebo, we might say ‘Treatment A is more effective than Placebo.’
Now, let’s say you have a further experiment, where one group gets Treatment A and another group gets a 3rd treatment, Treatment C (we might even have Waitlist Control D, to control for regression to the mean). And in this experiment, more patients who received Treatment C, had a 50% reduction in migraine than those receiving Treatment A.
So using a very simple model of internally consistent logic (applying what is known in geeky math-speak as Transitive Law), we would say that, by definition, Treatment C works better than placebo. If A is better than placebo and C is better than A, C is also better than placebo. If pharmaceuticals are better than placebo and acupuncture is better than pharmaceuticals, acupuncture is better than placebo. This is how logic works.
‘But, Mel,’ you say, ‘complex physical interventions have larger placebo effects than pills. In theory, acupuncture could work better at preventing migraine than sugar pill and the real drug and still be a theatrical placebo. Sure, in adequately powered trials, acupuncture does significantly outperform sham needling, but only by a little. This difference could be completely down to lack of blinding of the practitioner.’
Sure, that’s a possibility. But is that the most likely explanation based on the evidence? Are acupuncture’s results for reducing migraines consistent with other placebos? What the heck do we know about placebos anyway?
There seems to be a lot of misunderstanding around what placebos are and how to accurately tease out their effects from other specific and non-specific phenomena10 but there are two things that we do know: “In reality, placebos don’t do much; their effects tend to be small in magnitude and short in duration.” 11
Small in magnitude and short in duration. In other words, placebos have small effect sizes and only work in the short-term. A 2010 Cochrane systematic review of placebo treatments for all conditions supports this first point. They found that compared to no-treatment, placebos were associated with small effect sizes.12 In contrast, for migraine prevention, acupuncture is associated with moderate to large effects. Whether the outcome measure is headache frequency, responder rate, migraine attacks or migraine days, unlike a placebo, acupuncture demonstrates large effect sizes compared to no treatment.13
The placebo review also found that compared to no-treatment, sham-acupuncture needling has large effect sizes, whereas other sham treatments like TENS, had little to no effect. This data supports the contention of experts that sham-needling is not a placebo or inert sham control14 and that the difference between acupuncture and sham-needling is not the measure of its true effect size.15
We also know from research into placebos that they only work in the short-term; this finding is equally true for migraine reduction. A recent systematic review and meta-analysis looked at the effects of placebo for migraines in 78 studies that included 4,579 episodic migraine sufferers randomized to placebo. Before treatment, these patients averaged 5.3 headaches/month. After taking the placebo, they had a significant reduction in headache frequency one month into the study that persisted at 12 weeks. However, by weeks 16, 20, and 24, the patients were having just as many headaches as before.16
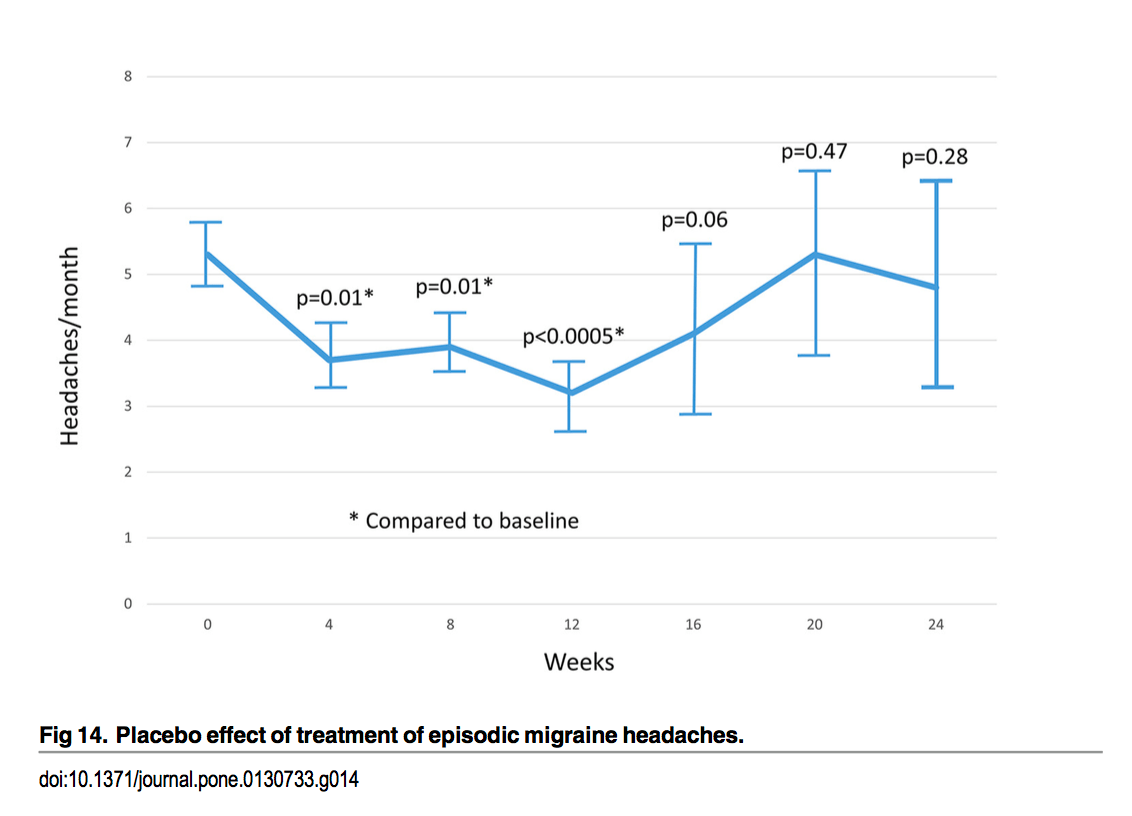
Jackson, J. L., Cogbill, E., Santana-Davila, R., & Eldredge, C. (2015). A comparative effectiveness meta-analysis of drugs for the prophylaxis of migraine headache. PLoS ONE. http://doi.org/10.1371/journal.pone.0130733.s001
In contrast, acupuncture has significant effects compared with no treatment, sham needling and drug-intervention at 3-4 month follow-up.17 Likewise, a recent review found that the majority of acupuncture’s clinical effects are maintained one year after treatment.18
So looking at this again, placebos and shams have small effects over no treatment and only work in the short term. Acupuncture has large effects over no treatment and its clinical effects persist in the long-term.
Applying that internally consistent logic thingy again, wouldn’t you have to conclude that acupuncture is not a placebo? Especially if you decide to include all the evidence and look at all that ‘irrelevant’ basic science research?
You seem to argue that, despite the basic science research demonstrating mechanisms through mechanotransduction and other neurological and biochemical effects of acupuncture needling, that acupuncture’s superiority to drugs is still fully placebo and other non-specific effects. It’s just an uncharacteristically large and long-acting, perhaps paradoxical and unique, placebo, which sounds a little bit like special pleading (a practice that uninterested and unbiased parties don’t tend to engage in).
No matter how you slice it, meta-analyses demonstrate that whatever acupuncturists are offering, it’s working as well as, if not better and more safely than, the alternatives when it comes to migraine prevention. If it’s not down to empathy, then what is it? How is it that acupuncture, which you argue is a placebo, outperforms conventional treatment? Which itself outperforms placebo? Which brings us to the virtue of ‘ethics’ in making recommendations. But first, let’s look at Virtue Number 3.
‘Intellectually thorough, rigorous and methodical’
Yep, this also sounds good. If it were available in a 12 oz can, I’d happily chug the whole thing.
So let’s be intellectually thorough, rigorous and methodical about reasonable treatment options for migraine prophylaxis. From my understanding, your main objection is that acupuncture doesn’t work because there’s no such thing as Qi or channels. Hopefully, that’s a fair categorization. If it’s not, no doubt you can clarify your position.
Assuming that’s a fair categorization, then let me clarify something first. If what you’re saying is that there isn’t an invisible ‘life force energy’ that flows through some as yet undiscovered physical structure referred to as a ‘channel’, I’m actually with you on that. That description simply isn’t a good translation or characterization of the Chinese medical model and certainly not been what’s discussed at any research conferences that I’ve attended.
However, if we’re going to take a stab at being ‘methodical,’ answer me this: can you explain the logic involved in the position that despite copious clinical research to the contrary, acupuncture doesn’t work because there’s no such thing as an invisible life force energy? Isn’t it possible that there’s no invisible, hitherto undiscovered life force energy AND AT THE SAME TIME acupuncture is effective at reducing migraines, as the best evidence supports?
Apparently, claiming that if an argument for some conclusion is fallacious, then the conclusion is false, is known as the ‘fallacy fallacy.‘ I love the way you skeptics name these things! Now, just because your position contains false logic, doesn’t in itself mean that acupuncture is effective for migraine prevention (that would actually be the ‘fallacy fallacy fallacy’, I kid you not). No, for that we have clinical research.
However you slice it, arguing that something doesn’t work despite ample evidence to the contrary because you perceive the model used to explain how it works as inaccurate isn’t exactly intellectually thorough, rigorous or methodical (if not downright logically fallacious!)
This faulty reasoning reminds me of a video I recently watched about a new light that runs on a kinetic motor so it’s powered simply using a weight and some gravity. (How frickin’ cool is that!) This one item is revolutionizing lives and allowing people in remote villages to have reliable access to light without the use of expensive and harmful kerosene.
In some regions of Kenya where the light is being distributed, the villagers, not understanding the mechanics of how the light works off the grid, are said to believe that it works using ‘supernatural power.’
If this situation were analogous to your current arguments about acupuncture, you’d be saying that the light doesn’t work because it can’t work since there’s no such thing as supernatural forces, even though everyone can clearly see that it does work (but perhaps then you’d be arguing that they just think they see light, that it’s another example of post hoc ergo propter hoc. I mean, just because they turned on the light and things got brighter, doesn’t mean that turning on the light caused illumination), not to mention that we can measure the photons it emits and that other explanations, consistent with dominant models explain how it works, at least to the extent that most drugs are understood. Such an argument would be clearly nonsensical. Whether or not the light works has nothing to do with whether the villagers explain that it works via these supernatural powers or not.
And there’s also the possibility, since we’re being thorough and rigorous in our approach and examining the phenomenon from all sides, that the villagers aren’t actually simpletons who lack the intellectual rigor to understand how the light works. It’s possible that the villagers speak a rare and poorly understood dialect of their language and that the people translating those explanations into English didn’t understand what the villagers were actually saying and mis-represented their position, making them look ‘pre-scientific’ and ‘superstitious’. It’s possible that a more accurate and nuanced, albeit less popular, translation of their worldview demonstrates a perspective that’s remarkably prescient and perhaps even includes models that have better explanatory power than the ones most widely used in conventional medicine. <Cue eye-rolls>
Let me anticipate your next objection: that if acupuncture doesn’t work by accessing ‘life force energy’ in ‘channels’ than those who are describing it as such are misleading the public and committing fraud. Or in your words: “it is misleading to say that such mechanisms (purinergic signaling, nitric oxide release, phosphorylation of collagen, etc) could explain “acupuncture.” Acupuncture is the needling of acupuncture points to affect the flow and balance of chi. Using needles to mechanically produce a temporary local counter-irritation effect is not acupuncture.”
Well, not to be whatever, but who died and made ‘Science Based Medicine’ the Supreme Arbiter of acupuncture definitions? This is a classic argumentum ad dicitonarium fallacy and very unscientific. Wouldn’t you be less at risk of being mistaken on this issue if you asked, for example, some of your tens of thousands of colleagues who are dually trained MDs and acupuncturists? Sure, it’s possible that all of them suffered brain aneurysms after medical school (oy, the stress!) and lost their ability to think critically. But you might just find that you have a lot more common ground than you’d expect and it’s also possible, if not probable, that those who have trained in acupuncture are in a better position to discuss definitions than those simply looking at ways to discredit it. It is simply incorrect to say that there is one, singular definition of acupuncture that relies on scientifically unvalidated concepts. The only reason for making such a claim is to disprove it, which not only reflects a strong bias, but one that prevents joining understanding with empiricism. Which leads us to the next ‘virtue’ in your shiny, ‘science-based’ halo.
‘Reasonably fair and unbiased in judgments’

Science, and the medicine it’s based on, should be reasonably fair and unbiased in judgments.
This point is another that sounds wonderful in theory but may be a bit hard to demonstrate its validity in practice. From where I’m sitting, science can’t make judgments. Only people can do that. And furthermore, science demonstrates that the study of science is biased and that the best we can do is be intellectually honest and aware of our biases in order to minimize them and do the best by our patients.19
Let’s say for example, that your intention is to improve public health by informing patients about their treatment options and drawing attention to the problems with certain treatments, using science and research. If that’s the goal, then can you explain any reason why your top priority wouldn’t be drawing attention to and recommending against the treatments that have the poorest benefit to harm ratios first? Why would you start with treatments that consistently demonstrate a superior benefit to harm profile, which you hypothesize is due to placebo and that basic science research demonstrates is due to mechano-transduction, rather than treatments that usually don’t work and have really nasty side-effects?
Is there a possibility that by choosing to focus on and criticise treatments with demonstrated effectiveness that seem illogical and silly to you (but not to the majority of your colleagues), that you might possibly be encouraging the use of more dangerous, and less effective treatments? And that this might be arising from the mistaken (and unscientific) belief that you can be unbiased? That you’re communicating a scientific perspective rather than spreading the good Gospel of Science?
Or we can put it another way. Your bias is that we shouldn’t recommend treatments based solely on demonstrated effectiveness and efficacy as Evidence Based Medicine suggests; treatments should also have known mechanisms and a reasonable level of prior plausibility, a measure that in itself is highly subjective. That’s your prerogative but isn’t that something that patients should get to decide for themselves?
From familiarizing myself with your work, the biggest assumption that I’ve seen you repeat without testing is this idea that there even are ‘treatments that work’ and ‘treatments that don’t’ in any absolute sense. If that’s a fair categorization, that you believe that a treatment can ‘work’ in an absolute binary sense, rather than a comparative ‘at a population level, the group that had this treatment had significantly better results than the other group but not so good as this 3rd group and none of this tells us how my patient, Jane Smith, is going to do on this treatment’, are you able to provide scientific support for this viewpoint? On the basis of what evidence are you supporting this theory of absolute, rather than relative, effectiveness?
Let’s look at an example.
A recent systematic review looked at responder rates amongst various drugs commonly used for migraine prevention, where a responder was defined as someone who had at least a 50% reduction in their migraines. Even amongst the drugs that had significantly more responders than placebo pill, none of them achieved a response in greater than half of those who took them. In other words, if you say that a drug ‘works’ in some sort of theoretical absolute Platonic sense when it significantly outperforms placebo, by that definition these drugs ‘work.’ But the best research also shows that when given to a group of migraine patients, they usually don’t work. So even migraine drugs that ‘work’ usually don’t work. How does that work? How does that work with the whole ‘internally consistent logic’ thing?
Now again, I honestly don’t know what the ‘Science-based’ recommendation is for migraine prophylaxis and I’m eager to hear what it is and what evidence this is based on. But systematic reviews and medical guidelines tend to conclude something like this: “Selection of prophylactic medication should be tailored according to patient preferences, characteristics and side effect profiles.” 20 If that does indeed echo your position, then on what basis can you recommend these treatments as science-based? Unless you’re now broadening your definition of science-based medicine to include the old n=1 ‘none of these drugs work particularly well and all of these have pretty nasty side-effects so let’s just try something and see how we get on?’
On the same token, the most recent Cochrane systematic review demonstrates that acupuncture has greater than 50% responder rate, or in other words, acupuncture usually works for migraine prevention (by ‘works’, I mean both that in systematic reviews of randomised controlled trials, patients with migraines who have acupuncture are more likely to be a responder than those who don’t in a way statistically unlikely due to chance and comparatively, patients who receive acupuncture have better results than those who receive drugs). I know that your position is that this is due to placebo rather than mechanano-transduction, purinergic signaling, and CGRP regulation, but are you sure that recommending a trial and error approach of treatments that usually don’t work and have unpleasant and often dangerous side-effects over a treatment that usually works and is very safe represents a ‘reasonably fair and unbiased judgment’ and puts patient safety and results over theory and your own personal beliefs?
‘Adheres to standards of ethics and professionalism’

Science Based Medicine consistently takes the position that offering placebos to patients, even without deception, is unethical. Personally, I believe that medical ethics (and the law) indicate that patients have a right to informed consent, including knowing when a treatment with a worse benefit to harm profile is out performed by a treatment that you call a placebo.
But let’s leave the ethics of prescribing placebos aside for a moment and let me ask you a different question. What are the ethics of prescribing a treatment that is inferior to placebo? If acupuncture is just a placebo and outperforms conventional pharmaceuticals, which have their own significant placebo built right in, then doesn’t internally consistent logic tell us quite clearly that these treatments are not only not helping but causing overt harm to patients?
Aside from the harm of not being as effective as acupuncture, these treatments used for migraine prophylaxis come with other harms that are relevant to a discussion of what Science Based Medicine recommends for these patients.
A recent review of prophylactic drugs for migraine found the following: “Drowsiness was the most common side effect, increased among patients taking gabapentin, pizotifen, topiramate, TCA and valproate. Tricyclic antidepressants also caused dry mouth and weight gain. Beta-blockers were associated with feeling depressed, dizzy and insomnia. Topiramate increased rates of nausea and paresthesia. Pizotifen had marked increased rates of weight gain with participants averaging 4.3 kg.”21 Of course, medical treatment isn’t all about the harm it can cause as all treatment carries some risk. However, the balance between benefits and harms of preventative migraine drugs is a poor one, leading to frequent discontinuation.
While NSAIDs were not included in the above Jackson review, the JAMA summary of migraine prevention does mention them based on a clinical guideline from the American Academy of Neurology22. While it’s nice to include NSAIDs, presumably to increase the number of options as there’s no evidence that they work, they’re not without their risks. They can cause everything from peptic ulcer and GI bleeding, to hepatitis, cirrhosis, renal stenosis, congestive heart failure, and asthma.23 According to one review in the United States, regular NSAID use causes 200,000-400,000 hospitalizations from upper GI disease a year with an annual cost of 0.8-1.6 billion dollars.24 These staggering figures don’t even include the incidence and cost of heart attacks caused by NSAIDs. A recent review found that taking any dose of NSAIDs for even short periods was associated with an increased risk of heart attack.25 Of course all of this makes sense, since the prostaglandins that NSAIDs lower actually do kind of important things in the body, like protect the gastric mucosa, regulate renal blood flow, support healthy lung function and regulate vasoconstriction and platelet aggregation. So based on how they work, we wouldn’t really expect them to be safe.
In contrast to acupuncture which is considered safe in pregnancy,26 none of the pharmaceutical preventatives are considered to be safe, as they can lead to congenital malformations, miscarriage and seizures in newborns.
To be sure, just because there aren’t any overwhelmingly effective or safe pharmaceutical treatments for migraine prevention doesn’t necessarily mean that acupuncture works; the evidence for that comes from systematic reviews of clinical trials. But if you’re choosing amongst treatments that don’t ‘work’ anyways, shouldn’t you at least be recommending the safest ones first? Especially when they work better than the more dangerous ones? Or is that somehow inconsistent with the ‘Science-based’ medical model?
Wrap up
“In theory, theory and practice are the same. In practice, they’re not.” Attributed to Albert Einstein, Yogi Berra, and others.
Looking at the practice of acupuncture as a whole, I will concede that there’s great heterogeneity in treatment styles and it would be interesting, if not useful, to study which techniques, theories and aspects of treatment work best, particularly in a way that is faithful to actual practice. I will also concede that while many Chinese medical theories are clinically useful and are consistent with modern science, some descriptions and understandings may be past their sell-by date or are based on a misunderstanding of the original theory. Just like with conventional medicine or any category of thought, we find the good, the bad, and the ugly; logic nor science supports equating any category with the worst that one can find within it (known as the ‘fallacy of composition‘).
That said, when it comes to migraine prevention, acupuncture clearly works, both in the ‘absolute’ sense (those who have acupuncture are more likely to have a significant reduction in migraine than those who don’t, unlike those who take pharmaceutical treatments for migraine) and in the more relevant, relative sense (acupuncture is more effective than pharmaceuticals, usual care, and sham needling for migraine prevention).27
It also doesn’t share the defining clinical features of placebos, in that unlike placebos, which only have small effects compared to no treatment and only work in the short-term, acupuncture has large effects compared to no treatment and has meaningful long-term clinical effects. It doesn’t walk or talk like a placebo; thus, it ain’t no placebo.
In light of the above, it may be worthwhile to review what makes science ‘scientific’? What are science’s defining characteristics?
In his internationally best-selling book ‘Sapiens’, Yuval Noah Harari’s explains that:
“modern science differs from all previous traditions of knowledge in . . . critical ways:
a. The willingness to admit ignorance. Modern science is based on the Latin injunction ignoramus – ‘we do not know’. It assumes that we don’t know everything. Even more critically, it accepts that the things that we think we know could be proven wrong as we gain more knowledge. No concept, idea or theory is sacred and beyond challenge.
b. The centrality of observation and mathematics. Having admitted ignorance, modern science aims to obtain new knowledge. It does so by gathering observations and then using mathematical tools to connect these observations into comprehensive theories.”28
If there’s any truth to the above, then Science Based Medicine’s focus verging on obsession with prior plausibility is actually completely unscientific. Rather than admit that we don’t know and then use empiricism to understand what’s happening in the world and make new theories, the prior plausibility of Science Based Medicine starts by saying ‘aren’t we clever, we may not know everything but we know enough’ and then uses this view to argue with, rather than understand, the data. The numbers say that patients get better with acupuncture compared to meds and that they’re put at far less risk of harm in the process. Let us tell you why the numbers are wrong according to our prior models.
The fact that science is based on the foundation of our awareness of our own ignorance is not a get out of jail free card to explain anything and everything as ‘possible’ or ‘scientific’. It is, however, a helpful reminder in the context of systematic reviews of thousands of randomised patients demonstrating an effective treatment for a common, debilitating condition for which satisfactory treatment options are scarce.
I hope you don’t mind all the questions and I’m really looking forward to increasing my knowledge of the Science Based Medicine approach to treating a clinical condition like migraine. From reading your blog and watching your videos, it was hard not to get the impression that you were more inclined to recommend treatments that don’t work well because you felt they should work in theory and recommend against treatments that do work, such as acupuncture, because in theory you felt that they shouldn’t based on your own narrow definition, which would be pretty unhelpful for patients (not to mention unnecessary, unethical and dangerous!). But, I’m sure you’ll be able to enlighten us on all the Science-y nuance that we’ve hitherto lacked the rigor to grasp.
1 NICE National Institute for Health and Care Excellence. (2012). CG150. Headaches in over 12s: diagnosis and management. (No. CG150). NICE. Retrieved from nice.org.uk/guidance/cg150
2 McDonald, J. L., & Janz, S. (2017). The Acupuncture Evidence Project, 1–81. Retrieved from acupuncture.org.au/OURSERVICES/Publications/AcupunctureEvidenceProject.aspx
3 Langevin, H. M. (2014). Acupuncture, connective tissue, and peripheral sensory modulation. Critical Reviews in Eukaryotic Gene Expression, 24(3), 249–253.
4 Takano, T., Chen, X., Luo, F., Fujita, T., Ren, Z., Goldman, N., et al. (2012). Traditional Acupuncture Triggers a Local Increase in Adenosine in Human Subjects. The Journal of Pain, 13(12), 1215–1223. doi.org/10.1016/j.jpain.2012.09.012
5 Ma, S.-X., Lee, P. C., Anderson, T. L., Li, X.-Y., & Jiang, I. Z. (2017). Response of Local Nitric Oxide Release to Manual Acupuncture and Electrical Heat in Humans: Effects of Reinforcement Methods. Evidence-Based Complementary and Alternative Medicine : eCAM, 2017, 1–8. doi.org/10.1155/2017/4694238
6 Lin, D., La Pena, De, I., Lin, L., Zhou, S.-F., Borlongan, C., & Cao, C. (2014). The Neuroprotective Role of Acupuncture and Activation of the BDNF Signaling Pathway. International Journal of Molecular Sciences, 15(2), 3234–3252. doi.org/10.3390/ijms15023234
7 Lundeberg, T. (2013). Acupuncture mechanisms in tissue healing: contribution of NO and CGRP. Acupuncture in Medicine, 31(1), 7–8. doi.org/10.1136/acupmed-2013-010313
8 Harris, R. E., Zubieta, J.-K., Scott, D. J., Napadow, V., Gracely, R. H., & Clauw, D. J. (2009). Traditional Chinese acupuncture and placebo (sham) acupuncture are differentiated by their effects on μ-opioid receptors (MORs). NeuroImage, 47(3), 1077–1085. doi.org/10.1016/j.neuroimage.2009.05.083
9 McDonald, J. L., & Janz, S. (2017). The Acupuncture Evidence Project, 1–81. Retrieved from acupuncture.org.au/OURSERVICES/Publications/AcupunctureEvidenceProject.aspx
10 Manchikanti, L., Boswell, M. V., Kaye, A. D., Helm Ii, S., & Hirsch, J. A. (2017). Therapeutic Role of Placebo: Evolution of a New Paradigm in Understanding Research and Clinical Practice. Pain Physician, 20(5), 363–386.
11 Friends of Science in Medicine. Is there any place for acupuncture in 21st century medical practice? Downloaded from: scienceinmedicine.org.au/wp-content/uploads/2017/06/acupuncturereview.pdf
12 Hróbjartsson, A., & Gøtzsche, P. C. (2010). Placebo interventions for all clinical conditions. The Cochrane Database of Systematic Reviews, (1), CD003974. doi.org/10.1002/14651858.CD003974.pub3
13 Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., et al. (2016). Acupuncture for the prevention of episodic migraine. (K. Linde, Ed.). Chichester, UK: John Wiley & Sons, Ltd. doi.org/10.1002/14651858.CD001218.pub3
14 Appleyard, I., Lundeberg, T., & Robinson, N. (2014). Should systematic reviews assess the risk of bias from sham–placeboacupuncture control procedures? European Journal of Integrative Medicine, 6(2), 234–243. doi.org/10.1016/j.eujim.2014.03.004
15 Manchikanti, L., Boswell, M. V., Kaye, A. D., Helm Ii, S., & Hirsch, J. A. (2017). Therapeutic Role of Placebo: Evolution of a New Paradigm in Understanding Research and Clinical Practice. Pain Physician, 20(5), 363–386.
16 Jackson, J. L., Cogbill, E., Santana-Davila, R., & Eldredge, C. (2015). A comparative effectiveness meta-analysis of drugs for the prophylaxis of migraine headache. PLoS ONE. doi.org/10.1371/journal.pone.0130733.s001
17 Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., et al. (2016). Acupuncture for the prevention of episodic migraine. (K. Linde, Ed.). Chichester, UK: John Wiley & Sons, Ltd. doi.org/10.1002/14651858.CD001218.pub3
18 MacPherson, H., Vertosick, E. A., Foster, N. E., Lewith, G., Linde, K., Sherman, K. J., et al. (2016). The persistence of the effects of acupuncture after a course of treatment. Pain, 1–22. doi.org/10.1097/j.pain.0000000000000747
19 Ioannidis, J. P. A. (2005). Why Most Published Research Findings Are False. PLoS Medicine, 2(8), e124. doi.org/10.1371/journal.pmed.0020124
20 Jackson, J. L., Cogbill, E., Santana-Davila, R., & Eldredge, C. (2015). A comparative effectiveness meta-analysis of drugs for the prophylaxis of migraine headache. PLoS ONE. doi.org/10.1371/journal.pone.0130733.s001
21 Jackson, J. L., Cogbill, E., Santana-Davila, R., & Eldredge, C. (2015). A comparative effectiveness meta-analysis of drugs for the prophylaxis of migraine headache. PLoS ONE. doi.org/10.1371/journal.pone.0130733.s001
22 Holland, S., Silberstein, S. D., Freitag, F., Dodick, D. W., Argoff, C., Ashman, E., Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. (2012, April 24). Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. Lippincott Williams & Wilkins. doi.org/10.1212/WNL.0b013e3182535d0c
23 Bahadur, S., Keshri, L., & Pathak, K. (2011). Adverse Drug Reactions and Safety Considerations of NSAIDs: Clinical Analysis. Current Drug Safety, 6(5), 310–317.
24 Smalley, WE., Griffin, MR. The risks and costs of upper gastrointestinal disease attributable to NSAIDs. Gastroenterol Clin North Am 1996; 25(2): 373-96.
25 Bally, M., Dendukuri, N., Rich, B., Nadeau, L., Helin-Salmivaara, A., Garbe, E., & Brophy, J. M. (2017). Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ (Clinical Research Ed.), 357, j1909–13. doi.org/10.1136/bmj.j1909
26 Park, J., Sohn, Y., White, A. R., & Lee, H. (2014). The safety of acupuncture during pregnancy: a systematic review. Acupuncture in Medicine : Journal of the British Medical Acupuncture Society, 32(3), 257–266. doi.org/10.1136/acupmed-2013-010480
27 Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., et al. (2016). Acupuncture for the prevention of episodic migraine. (K. Linde, Ed.). Chichester, UK: John Wiley & Sons, Ltd. doi.org/10.1002/14651858.CD001218.pub3
28 Harari, Yuval N., and Derek Perkins. Sapiens: A brief history of humankind. London: Harvill Secker, 2014.

